- Submit a Protocol
- Receive Our Alerts
- Log in
- /
- Sign up
- My Bio Page
- Edit My Profile
- Change Password
- Log Out
- EN
- EN - English
- CN - 中文
- Protocols
- Articles and Issues
- For Authors
- About
- Become a Reviewer
- EN - English
- CN - 中文
- Home
- Protocols
- Articles and Issues
- For Authors
- About
- Become a Reviewer
A Tumor-admixture Model to Interrogate Immune Cell–dependent Tumorigenesis
Published: Vol 13, Iss 5, Mar 5, 2023 DOI: 10.21769/BioProtoc.4630 Views: 2781
Reviewed by: Ivan ShapovalovXiaoyu LiuAnonymous reviewer(s)

Protocol Collections
Comprehensive collections of detailed, peer-reviewed protocols focusing on specific topics
Related protocols
Murine Osteoblast and Osteoclast Co-culture on Demineralized Bone Paper for Bone Remodeling
Seema Amin [...] Jungwoo Lee
Jun 5, 2025 2196 Views
Assessing Human Treg Suppression at Single-Cell Resolution Using Mass Cytometry
Jonas Nørskov Søndergaard [...] James B. Wing
Aug 20, 2025 2879 Views
Isolation and Co-culture of Paneth Cells and Intestinal Stem Cells
Ryosuke Isotani [...] Toshimasa Yamauchi
Sep 20, 2025 3413 Views
Abstract
A rigorous determination of effector contributions of tumor-infiltrating immune cells is critical for identifying targetable molecular mechanisms for the development of novel cancer immunotherapies. A tumor/immune cell–admixture model is an advantageous strategy to study tumor immunology as the fundamental methodology is relatively straightforward, while also being adaptable to scale to address increasingly complex research queries. Ultimately, this method can provide robust experimental information to complement more traditional murine models of tumor immunology. Here, we describe a tumor/macrophage-admixture model using bone marrow–derived macrophages to investigate macrophage-dependent tumorigenesis. Additionally, we provide commentary on potential branch points for optimization with other immune cells, experimental techniques, and cancer types.
Keywords: CancerBackground
Evasion of anti-tumor immunity is now a well-established hallmark of cancer progression (Hanahan and Weinberg, 2011). Translation of fundamental concepts in tumor immunity has resulted in the development of immune checkpoint inhibitors that are highly efficacious in select oncological types (Xin et al., 2019; Robert, 2020). However, several types of malignancies do not respond, have intrinsic resistance, or develop secondary adaptive resistance to these therapies (Sharma et al., 2017; Jenkins et al., 2018; Schoenfeld and Hellmann, 2020). These issues have led to an outpouring of basic science and translational projects aimed at identifying additional molecular mechanisms by which cancer cells or infiltrating immune cells evade anti-tumor immunity, with the goal of developing novel immunotherapeutics (Fares et al., 2019; Karasarides et al., 2022). Here, we detail a published tumor/immune cell–admixture model (Liu et al., 2020; Noe et al., 2021), using tumor-associated macrophages as an example, that can serve as a useful tool to investigate the relative contributions of tumor-infiltrating immune cells in promoting cancer progression.
Tumor-associated macrophages (TAMs) are myeloid-derived immune cells that infiltrate into the tumor microenvironment to affect tumorigenesis (Mantovani et al., 1992; Noy and Pollard, 2014; Pan et al., 2020; Pittet et al., 2022). TAMs have both pro- and anti-tumor effector functions—their phagocytosis of cancer cells (Kamber et al., 2021), presentation of tumor-associated antigens (Asano et al., 2011), and activation of anti-tumor adaptive immunity play a critical role in the elimination of cancer cells (Modak et al., 2022). In contrast, TAMs can also promote tumorigenesis by suppressing phagocytic and antigenic innate immune responses (Barkal et al., 2019; Demaria et al., 2019; Zhou et al., 2020), as well as by inducing adaptive immune cell exhaustion (DeNardo and Ruffell, 2019; Singhal et al., 2019). Understanding the TAM-dependent contribution to tumor progression or regression is critical for identifying novel tumor immunotherapeutic strategies.
Several different tumor models have been developed to interrogate the effects of specific immune cell types in tumorigenesis. These protocols traditionally include the targeted depletion (Xiao and Jiang, 2014) or transgenic manipulation (McCubbrey et al., 2017) of the desired immune cell in the context of orthotopic or heterotopic tumors in xenograft or allograft models. The tumor-admixture model described herein is a heterotopic, allograft murine model using ex vivo differentiated/polarized bone marrow–derived macrophages (BMDMs) injected with tumor cell lines into congenic recipient mice. This admixture model has been shown to be an advantageous strategy to relatively easily determine gene-specific contributions to TAM-dependent tumor progression (Liu et al., 2020; Noe et al., 2021).
While this protocol was developed to investigate the ability of ex vivo interleukin-4 (IL-4) polarized pro-tumor TAMs to suppress anti-tumor immunity leading to enhanced tumor growth (Liu et al., 2020; Noe et al., 2021), this model can be used with other TAM phenotypes, different immune cell types, and additional experimental manipulations. A potential critique of this model includes the relative contribution of host-derived, tumor-infiltrating TAMs, which can be addressed by incorporating a targeted depletion strategy (Xiao, and Jiang, 2014). Adapting this model using anti-tumor TAMs (Liu et al., 2020; Noe et al., 2021) offers an interesting approach to understanding the mechanisms by which TAMs promote tumor regression. With rigorous optimization, other immune cell types that are critical regulators of tumorigenesis, such as neutrophils (Shaul, and Fridlender, 2019), dendritic cells (Wculek et al., 2020), or myeloid-derived suppressor cells (Veglia et al., 2021), could be adapted for use. Lastly, this model is highly amendable to the post-injection administration of small molecules or biologic inhibitors to further validate their importance as a clinically viable therapeutic (Zanoni et al., 2012; Noe and Mitchell, 2020). Altogether, this tumor-admixture model is a relatively straightforward, highly adaptable protocol to investigate immune cell–dependent cancer progression.
Materials and Reagents
0.70 μm filter
2 mL syringe
28 gauge needle
Falcon conical centrifuge tubes, 15 mL (Corning, catalog number: 352095)
Microcentrifuge tubes, 1.5 mL (Sigma Aldrich, catalog number: HS4323)
C57BL/6J mice, CD45.2+ donor (Jackson Laboratory, strain #: 000664)
B6.SJL mice, CD45.1+ congenic recipient (Jackson Laboratory, strain #: 002014)
Matrigel matrix basement membrane (Corning, catalog number: 354234)
CellStripper dissociation solution (Corning, catalog number: 25-056-CI)
Trypsin-EDTA, 0.05% (Gibco, catalog number: 25300062)
Phosphate-buffered saline (PBS) (Corning, catalog number: 21-040)
RPMI 1640 medium (Gibco, catalog number: 11-875-093)
Fetal bovine serum (FBS), heat-inactivated (Gibco, catalog number: 10-082-147)
10 cm tissue culture–treated plates (Corning, catalog number: CLS430167)
Trypan Blue solution (Gibco, catalog number: 15250061)
Lewis lung carcinoma cells (ATCC, catalog number: CRL-1642)
Note: As an example, we engrafted Lewis lung carcinoma cells; see Procedure section B for more information. Please utilize the previously described Bio-Protocol manuscripts for BMDM differentiation and culture of C57BL/6J CD45.2+ donor mice: Zanoni et al. (2012), Haag and Murthy (2021).
Equipment
Tabletop centrifuge (e.g., Kendro Sorval legend RT)
Microcentrifuge (e.g., Eppendorf refrigerated microcentrifuge 5415R)
Water bath at 37 °C (e.g., Thermo Scientific PRECISION water bath)
Incubator at 37 °C with 5% CO2 (e.g., Thermo Scientific HERACell 150i CO2 incubator)
Laminar flow hood (e.g., The Baker Company, SterilGARD class II biological safety cabinet)
Cell lifter (VWR, catalog number: 76036-006)
Digital calipers (VWR, catalog number: 62379-531)
Procedure
Preparation
Pre-warm RPMI 1640 medium, PBS, FBS, trypsin-EDTA, and CellStripper dissociation solution in a water bath set to 37 °C.
Thaw Matrigel matrix basement membrane on ice.
Tip: Matrigel can prematurely solidify at room temperature, so care must be taken to ensure it is maintained in a liquid state until immediately before use.
Make wash media: RPMI 1640 medium + 5% FBS.
Make injection solution: PBS + 5% FBS.
Tumor cell line collection
Wash plates twice with 10 mL of PBS and aspirate PBS after each wash.
Add 3 mL of trypsin-EDTA to each plate and place in incubator for 3–5 min.
Transfer cells to fresh Falcon tubes.
Wash plate twice with 5 mL of wash media and add wash to Falcon tubes.
Centrifuge at 350 × g for 5 min and aspirate supernatant.
Resuspend cell pellet with 10 mL of wash solution.
Repeat steps B5 and B6.
Filter cell suspension through a 0.70 μm filter into a fresh Falcon tube.
Count cells in Trypan Blue solution using a cell counter or other standard method.
Centrifuge at 350 × g for 5 min and aspirate supernatant.
Resuspend cells to 4 × 106 cells/mL in the Falcon tubes and place tumor cells on ice.
Tip: The tumor cell collection can be performed simultaneously with the BMDM collection (Section C) to increase efficiency and reduce the length of time the tumor cells are kept on ice.
Bone marrow–derived macrophage (BMDM) collection
In a laminar flow hood, wash plates twice with 10 mL of PBS and aspirate PBS after each wash.
Add 3 mL of CellStripper dissociation solution to each plate and place in the incubator for 3–5 min.
Gently lift BMDMs with a cell lifter and transfer cells to Falcon tubes.
Tip: Avoid aggressive scraping of BMDMs or using trypsin instead of cell stripper, as this causes reduced BMDM viability.
Wash plate twice with 5 mL of wash media and add wash to Falcon tubes.
Centrifuge at 350 × g for 5 min and aspirate supernatant.
Resuspend cell pellet with 10 mL of wash solution.
Repeat steps C5 and C6.
Filter cell suspension through a 0.70 μm filter into a fresh Falcon tube.
Count cells in Trypan Blue using a cell counter or other standard method.
Centrifuge at 350 × g for 5 min and aspirate supernatant.
Resuspend cells to 1.6 × 106 cells/mL in the Falcon tubes and place BMDMs on ice.
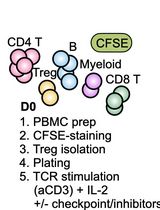
Tumor-BMDM admixture
Mix tumor cell suspension, aliquot 500 μL to fresh microcentrifuge tube, and place on ice.
Mix BMDM suspension, aliquot 500 μL to the same microcentrifuge tube, mix well, and place on ice.
Immediately prior to injection, aliquot 1 mL Matrigel to the microcentrifuge tube, mix well, and place on ice.
Draw 500 μL of the admixture into a 2 mL syringe and place a 28 gauge needle.
Tip: Again, Matrigel can prematurely solidify at room temperature. Pre-chilling syringes on ice before drawing admixture and placing syringe on ice in between injections may be needed.
Administer a 500 μL subcutaneous injection into the flank of a B6.SJL recipient mouse.
Tip: The flank can be shaved prior to injection to increase visibility during injection or subsequent measurements. Following injection, leave the needle in place for 1–3 s to prevent leakage from the insertion site. Any significant leakage should be noted and may represent a failed injection.
Using a new syringe, repeat steps D4 and D5 for each sequential mouse.
Downstream analyses
Monitor mice for tumor outgrowth to indicate a successful injection.
Once tumors are palpable (approximately day 5–7), measure the tumor length and width every 2–3 days with external calipers.
Record the length and width to calculate the tumor volume using the following formula: (length × width2)/2.
Once the tumor endpoint is reached, euthanize mice, resect tumors, and measure weight (Figure 1).
Proceed with downstream analyses, if desired.

Figure 1. Tumor-admixture model enhances tumor outgrowth. Gross dissection of tumors from mice 16 days post-injection with Lewis lung carcinoma (LLC) cells plus M2-polarized bone marrow–derived macrophages (BMDMs) (above) or LLC cells alone (below). Size differences represent variability of tumor size within each cohort. Please refer to Noe et al. (2021) for a more comprehensive analysis of tumor growth curves and endpoint tumor weight.- Almeida, A. S., Fein, M. R. and Egeblad, M. (2021). Multi-color Flow Cytometry for Comprehensive Analysis of the Tumor Immune Infiltrate in a Murine Model of Breast Cancer. Bio-protocol 11(11): e4012.
- Asano, K., Nabeyama, A., Miyake, Y., Qiu, C. H., Kurita, A., Tomura, M., Kanagawa, O., Fujii, S. and Tanaka, M. (2011). CD169-positive macrophages dominate antitumor immunity by crosspresenting dead cell-associated antigens. Immunity 34(1): 85-95.
- Barkal, A. A., Brewer, R. E., Markovic, M., Kowarsky, M., Barkal, S. A., Zaro, B. W., Krishnan, V., Hatakeyama, J., Dorigo, O., Barkal, L. J., et al. (2019). CD24 signalling through macrophage Siglec-10 is a target for cancer immunotherapy. Nature 572(7769): 392-396.
- Demaria, O., Cornen, S., Daeron, M., Morel, Y., Medzhitov, R. and Vivier, E. (2019). Harnessing innate immunity in cancer therapy. Nature 574(7776): 45-56.
- DeNardo, D. G. and Ruffell, B. (2019). Macrophages as regulators of tumour immunity and immunotherapy. Nat Rev Immunol 19(6): 369-382.
- Erstad, D. J., Sojoodi, M., Taylor, M. S., Ghoshal, S., Razavi, A. A., Graham-O'Regan, K. A., Bardeesy, N., Ferrone, C. R., Lanuti, M., Caravan, P., et al. (2018). Orthotopic and heterotopic murine models of pancreatic cancer and their different responses to FOLFIRINOX chemotherapy. Dis Model Mech 11(7): dmm034793.
- Fares, C. M., Van Allen, E. M., Drake, C. G., Allison, J. P. and Hu-Lieskovan, S. (2019). Mechanisms of Resistance to Immune Checkpoint Blockade: Why Does Checkpoint Inhibitor Immunotherapy Not Work for All Patients? Am Soc Clin Oncol Educ Book 39: 147-164.
- Haag, S. and Murthy, A. (2021). Murine Monocyte and Macrophage Culture. Bio-protocol 11(6): e3928.
- Hanahan, D. and Weinberg, R. A. (2011). Hallmarks of cancer: the next generation. Cell 144(5): 646-674.
- Jenkins, R. W., Barbie, D. A. and Flaherty, K. T. (2018). Mechanisms of resistance to immune checkpoint inhibitors. Br J Cancer 118(1): 9-16.
- Kamber, R. A., Nishiga, Y., Morton, B., Banuelos, A. M., Barkal, A. A., Vences-Catalan, F., Gu, M., Fernandez, D., Seoane, J. A., Yao, D., et al. (2021). Inter-cellular CRISPR screens reveal regulators of cancer cell phagocytosis. Nature 597(7877): 549-554.
- Karasarides, M., Cogdill, A. P., Robbins, P. B., Bowden, M., Burton, E. M., Butterfield, L. H., Cesano, A., Hammer, C., Haymaker, C. L., Horak, C. E., et al. (2022). Hallmarks of Resistance to Immune-Checkpoint Inhibitors. Cancer Immunol Res 10(4): 372-383.
- Liu, M., Tong, Z., Ding, C., Luo, F., Wu, S., Wu, C., Albeituni, S., He, L., Hu, X., Tieri, D., et al. (2020). Transcription factor c-Maf is a checkpoint that programs macrophages in lung cancer. J Clin Invest 130(4): 2081-2096.
- Mantovani, A., Bottazzi, B., Colotta, F., Sozzani, S. and Ruco, L. (1992). The origin and function of tumor-associated macrophages. Immunol Today 13(7): 265-270.
- McCubbrey, A. L., Allison, K. C., Lee-Sherick, A. B., Jakubzick, C. V. and Janssen, W. J. (2017). Promoter Specificity and Efficacy in Conditional and Inducible Transgenic Targeting of Lung Macrophages. Front Immunol 8: 1618.
- Modak, M., Mattes, A. K., Reiss, D., Skronska-Wasek, W., Langlois, R., Sabarth, N., Konopitzky, R., Ramirez, F., Lehr, K., Mayr, T., et al. (2022). CD206+ tumor-associated macrophages cross-present tumor antigen and drive antitumor immunity. JCI Insight 7(11).
- Noe, J. T. and Mitchell, R. A. (2020). MIF-Dependent Control of Tumor Immunity. Front Immunol 11: 609948.
- Noe, J. T., Rendon, B. E., Geller, A. E., Conroy, L. R., Morrissey, S. M., Young, L. E. A., Bruntz, R. C., Kim, E. J., Wise-Mitchell, A., Barbosa de Souza Rizzo, M., et al. (2021). Lactate supports a metabolic-epigenetic link in macrophage polarization. Sci Adv 7(46): eabi8602.
- Noy, R. and Pollard, J. W. (2014). Tumor-associated macrophages: from mechanisms to therapy. Immunity 41(1): 49-61.
- Pan, Y., Yu, Y., Wang, X. and Zhang, T. (2020). Tumor-Associated Macrophages in Tumor Immunity. Front Immunol 11: 583084.
- Pittet, M. J., Michielin, O. and Migliorini, D. (2022). Clinical relevance of tumour-associated macrophages. Nat Rev Clin Oncol 19(6): 402-421.
- Robert, C. (2020). A decade of immune-checkpoint inhibitors in cancer therapy. Nat Commun 11(1): 3801.
- Schoenfeld, A. J. and Hellmann, M. D. (2020). Acquired Resistance to Immune Checkpoint Inhibitors. Cancer Cell 37(4): 443-455.
- Sharma, P., Hu-Lieskovan, S., Wargo, J. A. and Ribas, A. (2017). Primary, Adaptive, and Acquired Resistance to Cancer Immunotherapy. Cell 168(4): 707-723.
- Shaul, M. E. and Fridlender, Z. G. (2019). Tumour-associated neutrophils in patients with cancer. Nat Rev Clin Oncol 16(10): 601-620.
- Singhal, S., Stadanlick, J., Annunziata, M. J., Rao, A. S., Bhojnagarwala, P. S., O'Brien, S., Moon, E. K., Cantu, E., Danet-Desnoyers, G., Ra, H. J., et al. (2019). Human tumor-associated monocytes/macrophages and their regulation of T cell responses in early-stage lung cancer. Sci Transl Med 11(479).
- Veglia, F., Sanseviero, E. and Gabrilovich, D. I. (2021). Myeloid-derived suppressor cells in the era of increasing myeloid cell diversity. Nat Rev Immunol 21(8): 485-498.
- Wculek, S. K., Cueto, F. J., Mujal, A. M., Melero, I., Krummel, M. F. and Sancho, D. (2020). Dendritic cells in cancer immunology and immunotherapy. Nat Rev Immunol 20(1): 7-24.
- Xiao, Z. and Jiang, Q. (2014). Protocol for Macrophage Depletion from Mice. Bio-protocol 4(11): e1144.
- Xin, Y. J., Hubbard-Lucey, V. M. and Tang, J. (2019). Immuno-oncology drug development goes global. Nat Rev Drug Discov 18(12): 899-900.
- Zanoni, I., Ostuni, R. and Granucci, F. (2012). Generation of Mouse Bone Marrow-Derived Macrophages (BM-MFs). Bio-protocol 2(12): e225.
- Zhou, J., Tang, Z., Gao, S., Li, C., Feng, Y. and Zhou, X. (2020). Tumor-Associated Macrophages: Recent Insights and Therapies. Front Oncol 10: 188.
Note: Most murine tumor cell lines are likely amendable to this model, but this should be predetermined by optimization studies using B6.SJL recipient mice. On the day of injection, tumor cells should be in 10 cm tissue culture plates and in log-growth phase (approximately 5.0 × 106–7.0 × 106). Although 5.0 × 105 tumor cells per injection is our recommended baseline, this number should be optimized based upon the cell line’s in vivo proliferation rate and desired time of tumor growth.
Note: BMDMs need to be derived from C57BL/6J CD45.2+ donor mice. The length of BMDM polarization prior to injection should be optimized based upon polarization method and experimental investigations (i.e., M1 vs. M2 polarization, small molecule inhibitor treatments, or transgenic manipulations). For example: we have used a transgenic model of BMDMs from C57BL/6J CD45.2+ donor mice that were polarized with IL-4 for 24 h (Noe et al., 2021). On the day of injection, BMDMs should have high viability (>90%), as determined by Trypan Blue exclusion, and 2.0 × 105 BMDMs per injection is needed.
Note: A limited optimization study should be performed beforehand to determine the preferred tumor cell:BMDM ratio. As a baseline, we have found that a 2.5:1 ratio provides meaningful data (Liu et al., 2020; Noe et al., 2021), but results may vary depending on tumorigenic potential, immunogenicity, and other experimental conditions. Each 2 mL tube can hold three tumor injections (1.5 mL injection + 0.5 mL slop; the required volume needed for tumor injections should be determined beforehand). For best results, the following steps should be performed immediately prior to injections. Currently, we describe a heterotopic model utilizing subcutaneous injections. In some cancer subtypes, different treatment responses occur depending on whether an orthotopic or heterotopic model is used (Erstad et al., 2018). We anticipate that this admixture model could be adapted to an orthotopic approach, but this will likely require thorough optimization beforehand.
Per 2 mL microcentrifuge tube: three injections (500 μL/injection) + 500 μL extra volume:
Note: Following injections, several experimental manipulations and/or downstream analyses are possible. The effect of a small molecule inhibitor or a biologic can be interrogated through the administration of these agents at predetermined time points. Once tumor endpoints are achieved, immunophenotyping with flow cytometry is possible by obtaining the spleen, blood, and tumor through previously described protocols (Almeida et al., 2021). At a minimum, tumor growth and end-point weight should be measured to determine gross changes in tumorigenesis, which are described below.
Acknowledgments
This work was supported by National Institutes of Health (NIH) Predoctoral Fellowship Award F30CA232550 (to J.T.N.), NIH Research Grant R01CA186661 (to R.A.M.), NIH Research Grant GB130096P3 (to R.A.M.), and NIH Project Grant P20GM135004 (to J.Y. and R.A.M.). This protocol is derived from the original research paper (Noe et al., 2021; DOI: 10.1126/sciadv.abi860).
Competing interests
The authors declare no competing interests.
Ethics
Animals were maintained under specific pathogen-free conditions and handled in accordance with the Association for Assessment and Accreditation of Laboratory Animals Care international guidelines. The Institutional Animal Care and Use Committee at the University of Louisville approved the experiments.
References
Article Information
Copyright
© 2023 The Author(s); This is an open access article under the CC BY-NC license (https://creativecommons.org/licenses/by-nc/4.0/).
How to cite
Readers should cite both the Bio-protocol article and the original research article where this protocol was used:
- Noe, J. T., Ding, C., Geller, A. E., Rendon, B. E., Yan, J. and Mitchell, R. A. (2023). A Tumor-admixture Model to Interrogate Immune Cell–dependent Tumorigenesis. Bio-protocol 13(5): e4630. DOI: 10.21769/BioProtoc.4630.
- Noe, J. T., Rendon, B. E., Geller, A. E., Conroy, L. R., Morrissey, S. M., Young, L. E. A., Bruntz, R. C., Kim, E. J., Wise-Mitchell, A. and M., Barbosa de Souza Rizzo (2021). Lactate supports a metabolic-epigenetic link in macrophage polarization. Sci Adv 7(46): eabi8602.
Category
Immunology > Animal model > Mouse
Cancer Biology > Tumor immunology > Tumor formation
Cell Biology > Cell isolation and culture > Co-culture
Do you have any questions about this protocol?
Post your question to gather feedback from the community. We will also invite the authors of this article to respond.
Share
Bluesky
X
Copy link