- EN - English
- CN - 中文
A Tumor-admixture Model to Interrogate Immune Cell–dependent Tumorigenesis
研究免疫细胞依赖性肿瘤发生的肿瘤混合模型
发布: 2023年03月05日第13卷第5期 DOI: 10.21769/BioProtoc.4630 浏览次数: 2781
评审: Ivan ShapovalovXiaoyu LiuAnonymous reviewer(s)
Abstract
A rigorous determination of effector contributions of tumor-infiltrating immune cells is critical for identifying targetable molecular mechanisms for the development of novel cancer immunotherapies. A tumor/immune cell–admixture model is an advantageous strategy to study tumor immunology as the fundamental methodology is relatively straightforward, while also being adaptable to scale to address increasingly complex research queries. Ultimately, this method can provide robust experimental information to complement more traditional murine models of tumor immunology. Here, we describe a tumor/macrophage-admixture model using bone marrow–derived macrophages to investigate macrophage-dependent tumorigenesis. Additionally, we provide commentary on potential branch points for optimization with other immune cells, experimental techniques, and cancer types.
Keywords: Cancer (癌症)Background
Evasion of anti-tumor immunity is now a well-established hallmark of cancer progression (Hanahan and Weinberg, 2011). Translation of fundamental concepts in tumor immunity has resulted in the development of immune checkpoint inhibitors that are highly efficacious in select oncological types (Xin et al., 2019; Robert, 2020). However, several types of malignancies do not respond, have intrinsic resistance, or develop secondary adaptive resistance to these therapies (Sharma et al., 2017; Jenkins et al., 2018; Schoenfeld and Hellmann, 2020). These issues have led to an outpouring of basic science and translational projects aimed at identifying additional molecular mechanisms by which cancer cells or infiltrating immune cells evade anti-tumor immunity, with the goal of developing novel immunotherapeutics (Fares et al., 2019; Karasarides et al., 2022). Here, we detail a published tumor/immune cell–admixture model (Liu et al., 2020; Noe et al., 2021), using tumor-associated macrophages as an example, that can serve as a useful tool to investigate the relative contributions of tumor-infiltrating immune cells in promoting cancer progression.
Tumor-associated macrophages (TAMs) are myeloid-derived immune cells that infiltrate into the tumor microenvironment to affect tumorigenesis (Mantovani et al., 1992; Noy and Pollard, 2014; Pan et al., 2020; Pittet et al., 2022). TAMs have both pro- and anti-tumor effector functions—their phagocytosis of cancer cells (Kamber et al., 2021), presentation of tumor-associated antigens (Asano et al., 2011), and activation of anti-tumor adaptive immunity play a critical role in the elimination of cancer cells (Modak et al., 2022). In contrast, TAMs can also promote tumorigenesis by suppressing phagocytic and antigenic innate immune responses (Barkal et al., 2019; Demaria et al., 2019; Zhou et al., 2020), as well as by inducing adaptive immune cell exhaustion (DeNardo and Ruffell, 2019; Singhal et al., 2019). Understanding the TAM-dependent contribution to tumor progression or regression is critical for identifying novel tumor immunotherapeutic strategies.
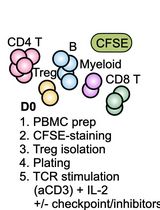
Several different tumor models have been developed to interrogate the effects of specific immune cell types in tumorigenesis. These protocols traditionally include the targeted depletion (Xiao and Jiang, 2014) or transgenic manipulation (McCubbrey et al., 2017) of the desired immune cell in the context of orthotopic or heterotopic tumors in xenograft or allograft models. The tumor-admixture model described herein is a heterotopic, allograft murine model using ex vivo differentiated/polarized bone marrow–derived macrophages (BMDMs) injected with tumor cell lines into congenic recipient mice. This admixture model has been shown to be an advantageous strategy to relatively easily determine gene-specific contributions to TAM-dependent tumor progression (Liu et al., 2020; Noe et al., 2021).
While this protocol was developed to investigate the ability of ex vivo interleukin-4 (IL-4) polarized pro-tumor TAMs to suppress anti-tumor immunity leading to enhanced tumor growth (Liu et al., 2020; Noe et al., 2021), this model can be used with other TAM phenotypes, different immune cell types, and additional experimental manipulations. A potential critique of this model includes the relative contribution of host-derived, tumor-infiltrating TAMs, which can be addressed by incorporating a targeted depletion strategy (Xiao, and Jiang, 2014). Adapting this model using anti-tumor TAMs (Liu et al., 2020; Noe et al., 2021) offers an interesting approach to understanding the mechanisms by which TAMs promote tumor regression. With rigorous optimization, other immune cell types that are critical regulators of tumorigenesis, such as neutrophils (Shaul, and Fridlender, 2019), dendritic cells (Wculek et al., 2020), or myeloid-derived suppressor cells (Veglia et al., 2021), could be adapted for use. Lastly, this model is highly amendable to the post-injection administration of small molecules or biologic inhibitors to further validate their importance as a clinically viable therapeutic (Zanoni et al., 2012; Noe and Mitchell, 2020). Altogether, this tumor-admixture model is a relatively straightforward, highly adaptable protocol to investigate immune cell–dependent cancer progression.
Materials and Reagents
0.70 μm filter
2 mL syringe
28 gauge needle
Falcon conical centrifuge tubes, 15 mL (Corning, catalog number: 352095)
Microcentrifuge tubes, 1.5 mL (Sigma Aldrich, catalog number: HS4323)
C57BL/6J mice, CD45.2+ donor (Jackson Laboratory, strain #: 000664)
B6.SJL mice, CD45.1+ congenic recipient (Jackson Laboratory, strain #: 002014)
Matrigel matrix basement membrane (Corning, catalog number: 354234)
CellStripper dissociation solution (Corning, catalog number: 25-056-CI)
Trypsin-EDTA, 0.05% (Gibco, catalog number: 25300062)
Phosphate-buffered saline (PBS) (Corning, catalog number: 21-040)
RPMI 1640 medium (Gibco, catalog number: 11-875-093)
Fetal bovine serum (FBS), heat-inactivated (Gibco, catalog number: 10-082-147)
10 cm tissue culture–treated plates (Corning, catalog number: CLS430167)
Trypan Blue solution (Gibco, catalog number: 15250061)
Lewis lung carcinoma cells (ATCC, catalog number: CRL-1642)
Note: As an example, we engrafted Lewis lung carcinoma cells; see Procedure section B for more information. Please utilize the previously described Bio-Protocol manuscripts for BMDM differentiation and culture of C57BL/6J CD45.2+ donor mice: Zanoni et al. (2012), Haag and Murthy (2021).
Equipment
Tabletop centrifuge (e.g., Kendro Sorval legend RT)
Microcentrifuge (e.g., Eppendorf refrigerated microcentrifuge 5415R)
Water bath at 37 °C (e.g., Thermo Scientific PRECISION water bath)
Incubator at 37 °C with 5% CO2 (e.g., Thermo Scientific HERACell 150i CO2 incubator)
Laminar flow hood (e.g., The Baker Company, SterilGARD class II biological safety cabinet)
Cell lifter (VWR, catalog number: 76036-006)
Digital calipers (VWR, catalog number: 62379-531)
Procedure
文章信息
版权信息
© 2023 The Author(s); This is an open access article under the CC BY-NC license (https://creativecommons.org/licenses/by-nc/4.0/).
如何引用
Readers should cite both the Bio-protocol article and the original research article where this protocol was used:
- Noe, J. T., Ding, C., Geller, A. E., Rendon, B. E., Yan, J. and Mitchell, R. A. (2023). A Tumor-admixture Model to Interrogate Immune Cell–dependent Tumorigenesis. Bio-protocol 13(5): e4630. DOI: 10.21769/BioProtoc.4630.
- Noe, J. T., Rendon, B. E., Geller, A. E., Conroy, L. R., Morrissey, S. M., Young, L. E. A., Bruntz, R. C., Kim, E. J., Wise-Mitchell, A. and M., Barbosa de Souza Rizzo (2021). Lactate supports a metabolic-epigenetic link in macrophage polarization. Sci Adv 7(46): eabi8602.
分类
免疫学 > 动物模型 > 小鼠
癌症生物学 > 肿瘤免疫学 > 肿瘤形成
细胞生物学 > 细胞分离和培养 > 共培养
您对这篇实验方法有问题吗?
在此处发布您的问题,我们将邀请本文作者来回答。同时,我们会将您的问题发布到Bio-protocol Exchange,以便寻求社区成员的帮助。
Share
Bluesky
X
Copy link